“It had finally worked out and I became pregnant with our little ‘polar bear’. Since yesterday, we are the proud parents of a healthy baby girl and we couldn’t be more thrilled.”
In this way or in a very similar one, couples talk about their experiences gained during IVF treatment involving a so-called ‘cryo cycle’. The procedure comprises the initial freezing of the embryo (fertilized oocyte in the early stages of its embryonic development) in order to thaw it at a later point in time and transfer it to the uterus (embryo transfer).
But why does the attending doctor opt for this kind of therapy?
During fertility treatment, situations may arise that require the freezing and storage (cryopreservation) of fertilized oocytes and embryos in specific development stages, for example, in cases where
… the endometrium has not developed adequately following the required hormonal stimulation. Thus, embryo transfer cannot be carried out, i.e. the uterus is not yet prepared for an immediate embryo replacement. As a consequence, adjustments must be made to the medication. Since this takes a certain amount of time and an embryo cannot be kept in culture that long, the embryo will be cryopreserved.
… the patient has developed ovarian hyper-stimulation syndrome (OHSS). A regimen of injectable hormone medications may, depending on dosage and disposition, cause a temporary but significant enlargement of the ovaries, which can, in turn, cause severe abdominal pain. This may additionally lead to fluid retention in the abdomen and lungs, causing shortness of breath and nausea. The condition also contributes to an increased risk of thrombosis. This is why embryo transfer is delayed and the doctor takes all the necessary measures to relieve the symptoms of OHSS. The existing embryos will be cryopreserved.
… it is intended to perform genetic investigations by means of PGD/PGS (for more details please see link “Genetics in the context of fertility Treatment”). In order to perform the relevant analysis, cell material is removed from the embryo (where appropriate – from the oocyte) prior to the transfer of this embryo to the uterus. This is referred to as ‘biopsy’. The embryo(s) remain(s) cryopreserved throughout the entire period during which genetic testing is carried out and until a decision on further proceedings has been taken after the laboratory result is available.
… no more than 1 embryo is transferred to the uterus (“Single Embryo Transfer”), in order to avoid multiple pregnancies which can pose serious health risks to both mother and child. In situations where – apart from the embryo(s) to be transferred (max. 2) – further embryos emerge from the treatment cycle, these embryos will be cryopreserved.
As to the examples stated above, it must be observed that any details on the therapeutic indication and legal frameworks as well as on the procedure and the possible risks involved will be clarified in a personal conversation with the doctor.
Cryopreservation – What happens in the laboratory?

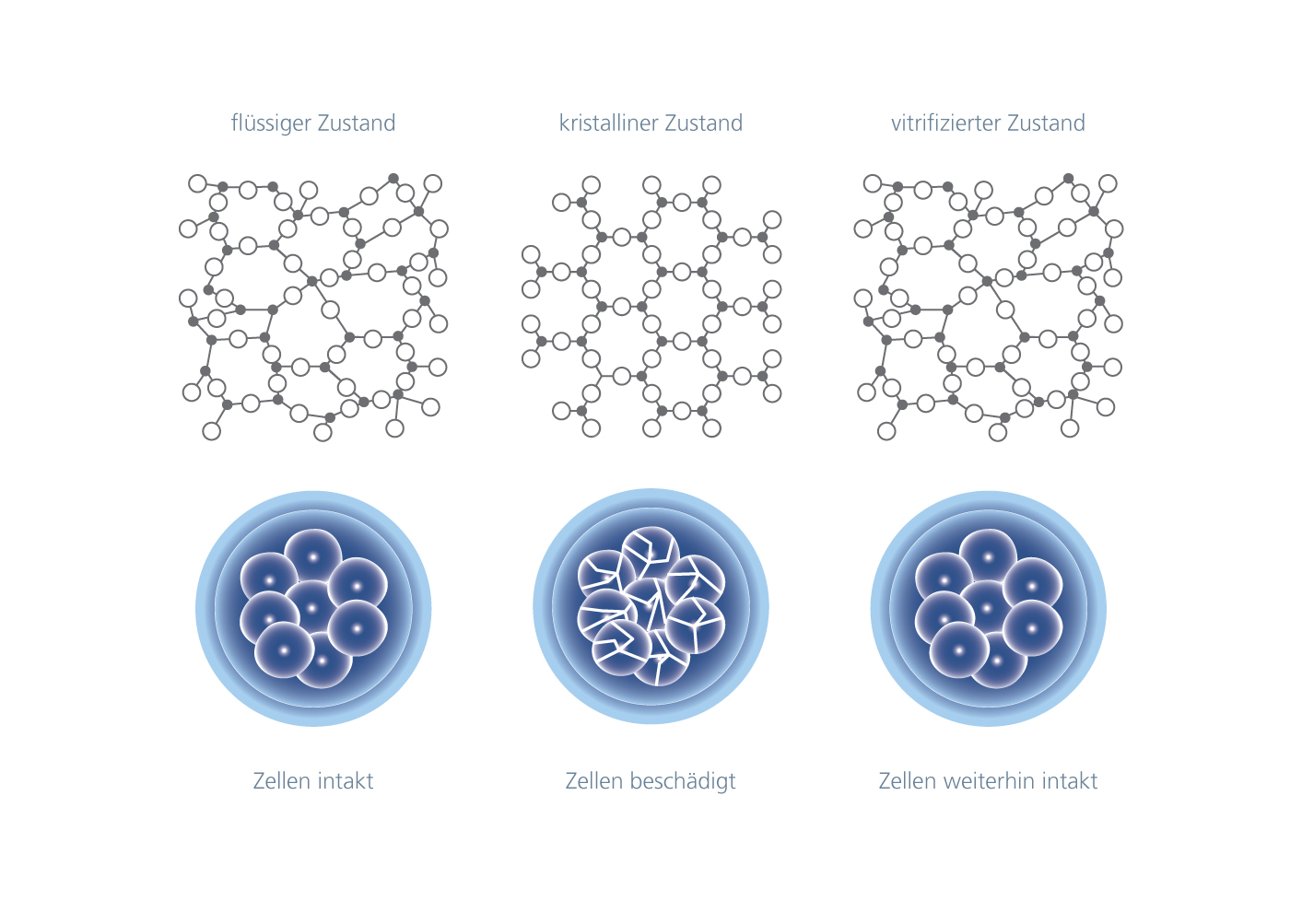
Human reproductive cells are cryopreserved at extremely low temperatures. Liquid nitrogen is used to reach such temperatures. Under these conditions, unfertilized oocytes, spermatozoa, fertilized oocytes and embryos may, for example, be stored for extended periods, without their biological function or viability being interfered with.
Aseptic vitrification is a modern and scientifically founded technique for cryopreservation. The cells are placed in a ‘closed’ carrier device (hermetically sealed system) to be frozen at -196°C before being stored in a nitrogen tank.
Vitrification means the transition to a glass-like state, i.e. the solidification of a solution without ice crystal formation. This is important because ice crystals damage the cells.
Internationally leading biologists and embryologists like Dr. Pierre Vanderzwalmen (→ publications) developed the vitrification technique. Since 1993, Dr. Vanderzwalmen has been a member of the team of the IVF Centers Prof. Zech, which was where the cryopreservation medium (effective composition), the cryo-straws and the procedure were first developed in order to be able to perform aseptic vitrification (VitriSafe®) of unfertilized oocytes, embryos and biopsied embryos (PGD/PGS).
In conclusion, there are various reasons why a couple’s medical situation may require individually tailored IVF treatment including a ‘cryo-cycle’. In order to increase the likelihood of achieving a successful pregnancy and the birth of a healthy child, it is crucial to ensure the safe use of modern cryopreservation techniques by an experienced medical and laboratory team.
Cryopreservation in Reproductive Medicine
Special cryopreservation procedures (e.g. vitrification) allow the safe freezing and storage of human reproductive cells:
- Spermatozoa
- Oocytes
- Fertilized oocytes
- Embryos in various stages of embryonic development (e.g. blastocyst)
Links:
» The Precautionary Freezing of Egg Cells
(Post | https://www.fertility-treatment-blog.com)
» Genetics in the context of fertility treatment
(Topic-Special | hhttps://www.fertility-treatment-blog.com)
(Start page | https://www.fertility-treatment-blog.com)
(Page | https://www.fertility-treatment-blog.com)