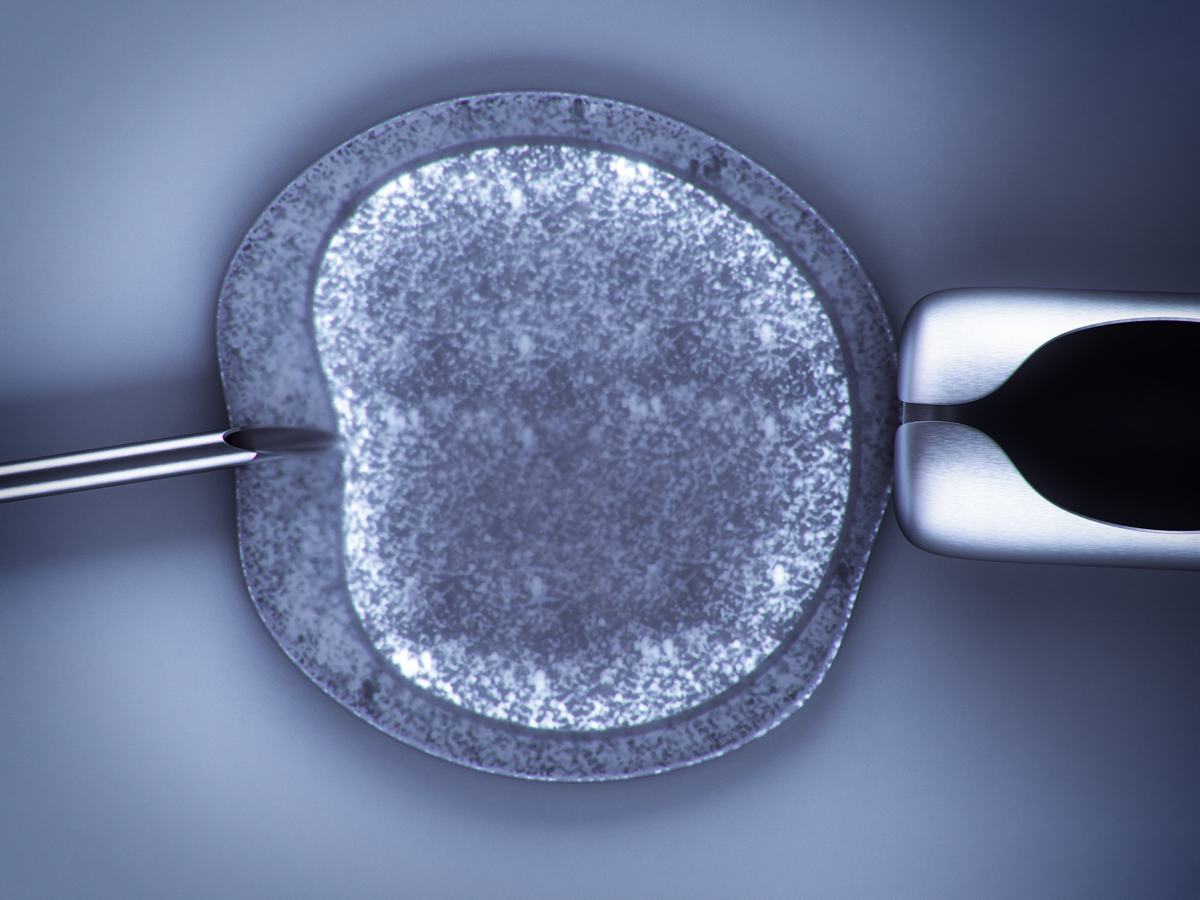
IVF treatment involves the fertilization of an oocyte by a sperm under the microscope. To this end, different techniques may be used, such as ICSI and IMSI. In order to learn more about the role played by these laboratory techniques in the assessment of sperm quality and subsequently also in a successful therapy outcome, we intend to closely examine the matter, while taking into account the findings of a recent study.
For the sake of a better understanding, we would like to start by briefly outlining the entire cycle of therapy. Controlled ovarian stimulation is the first step in IVF treatment. Follicle stimulating hormones are used to induce the development of multiple egg-containing follicles in a woman’s ovaries. Transvaginal oocyte retrieval is used to remove these oocytes from the ovaries. Subsequently, the quality of the collected oocytes is analyzed (diagnosis of oocyte quality). While the oocytes are being collected, the male partner is asked to produce a semen sample by masturbation. The obtained oocytes will thus be fertilized with the prepared sperm outside of the woman’s body in a laboratory procedure. In this context, there are several techniques, such as IMSI and ICSI which also serve the purpose of evaluating sperm quality (sperm diagnostics).
The fertilized oocytes are placed in a special media and cultured in an incubator until they have reached the blastocyst stage (blastocyst culture). Once the embryos have reached a particular stage of development (blastocyst = embryo capable of implantation), the embryo with the highest implantation potential is selected and transferred to the woman’s uterus (embryo transfer). Ideally, the embryo implants itself into the uterine wall, hopefully resulting in a successful pregnancy and the birth of a healthy child.
Difference between IMSI and ICSI
The IMSI technique (Intracytoplasmic Morphologically Selected Sperm Injection) is based on the real-time (“live”) analysis of sperm using a high-resolution microscope at a magnification of 6.000-12.000 times.
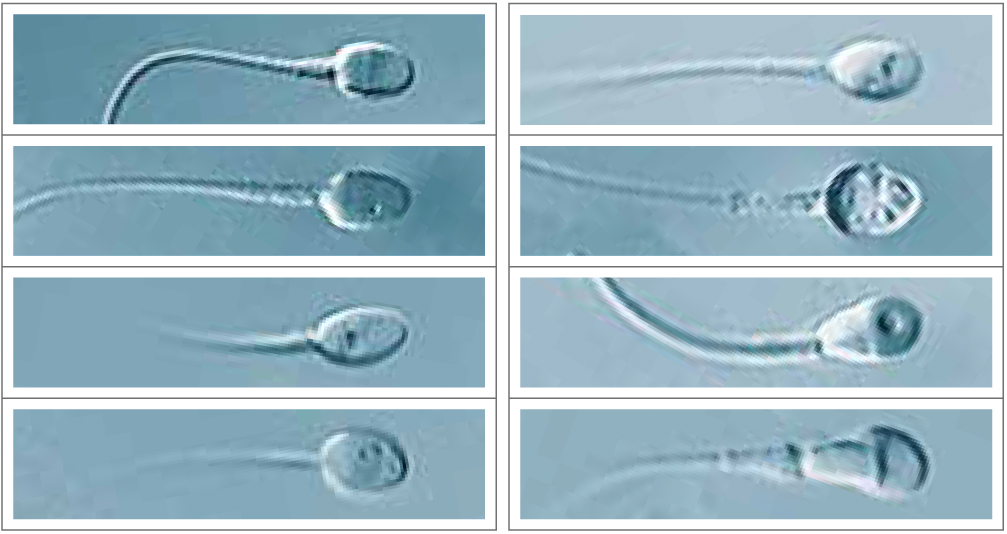

This technique also allows for the identification of tiny structural defects such as vacuoles (= crater-like dents on the nuclear surface). Even though the cause for the appearance of vacuoles has still not been fully clarified, their presence is associated with poor sperm quality. Numerous studies have proven a positive correlation between the selection of spermatozoa without nuclear vacuoles and a positive treatment outcome in couples facing infertility.
Conventional
Since the 1990s, there has always been ongoing research into the use of the IMSI technique. A great number of scientific papers have suggested that the use of IMSI may not only lead to improved IVF parameters [greater number of (top) blastocysts], but also to an improvement in clinical success parameters (e.g. higher pregnancy and implantation rates, lower miscarriage rates).
The risk of congenital malformations is deemed to be lower
But so far, very little has been known regarding a possible link between the use of IMSI and the likelihood of giving birth to a healthy child. In 2014, a study was published for the first time, suggesting a significantly lower risk for congenital malformations among children born after IMSI (see links).
Basically, these findings could be confirmed by a multi-center study published in early 2018. The study was conducted by the IVF Zentren Prof. Zech in close cooperation with the Centre de Procréation Médicalement Assistée – ULiège, Centre Hospitalier Universitaire de Liège. It investigated 275 ICSI- and 573 IMSI treatments which eventually resulted in pregnancy. The good news was that the percentage of malformation was low in both groups. Although no statistically significant difference could be observed, a trend towards a lower rate of congenital defects could be identified in the IMSI-group. These findings are in line with the aforementioned work and a further study by a group of Israeli scientists. The Israeli study, too, reported a lower risk of birth defects in children born after IMSI (see links).
To conclude, it can be said that, apart from the better “outcome” due to blastocyst culture and higher success rates following embryo transfer, the likelihood of giving birth to a healthy child may be higher after IMSI than after conventional ICSI.
Links:
» Low birth defects by deselecting abnormal spermatozoa before ICSI
(Study | https://www.ncbi.nlm.nih.gov)
» Impact of high magnification sperm selection on neonatal outcomes: a retrospective study
(Study | https://www.ncbi.nlm.nih.gov)
(Study | https://www.ncbi.nlm.nih.gov)
» Sperm quality – Assessment and significance in fertility treatments
(Post | https://www.fertility-treatment-blog.com/)
» Spermiogram – What’s possible nowadays when it comes to the assessment of male fertility
(Post | https://www.fertility-treatment-blog.com/)
(Start page | https://www.fertility-treatment-blog.com/)
(Page | https://www.fertility-treatment-blog.com/)